The role of calcium in building and maintaining healthy bones is well established, and dairy foods are recognised as important sources of calcium, supplying up to two thirds of intake in the European diet. However, milk and dairy foods also contain other nutrients needed for bone health including protein, phosphorus, potassium, magnesium, zinc and vitamin K2 (and vitamin D in the case of fortified dairy). The beneficial effects of dairy foods on bone may be greater than can be explained by any single nutrient they contain or even the sum of the nutrients, suggesting a synergistic or ‘matrix effect’. Increasingly, the science indicates that the nutrients and other components of the dairy matrix work together to help maintain healthy bones.
Dairy and bone health in children and adolescents
Both observational and intervention studies provide evidence linking dairy consumption with bone health in children and adolescents1-3. A meta-analysis of studies investigating the effect of dairy products and dietary calcium (predominantly from dairy) on bone mineral content (BMC) reported that total body and lumbar spine BMC were significantly greater in children with higher intakes4. Dairy as part of an overall healthy dietary pattern has also been associated with beneficial effects on bone development5. Intervention studies which have specifically used milk or dairy foods are limited compared with those for calcium supplements, but positive effects have been reported; including in French, Finnish and British children6-8. For example, significant improvements in bone mineral acquisition compared to control subjects were observed in adolescent British girls who were given 568ml (one pint) of milk a day for 18 months8. A systematic literature review of controlled trials which have assessed the effect of children’s dairy consumption on BMC, concluded that supplementing the usual diet with dairy foods increases BMC9. The corollary is that milk avoidance in children has been associated with increased risk of fracture and poorer bone health10,11. In a 2016 position statement on lifestyle choices that promote maximal bone health from childhood through adolescence, the National Osteoporosis Foundation concludes that there is ‘good evidence’ for a role for dairy consumption2. A number of retrospective studies, although not all, suggest that milk consumption in childhood and adolescence may be related to better bone health and / or reduced risk of fracture later in life12. There are limitations to such studies, however, including accurate recall of childhood milk and dairy intake.
Dairy and bone health in adults
For adults, the majority of observational studies report either a positive association between milk and milk products and BMC or bone mineral density (BMD) or a neutral outcome1,3. Again, randomised controlled trials using milk and dairy foods are limited compared with calcium supplementation ones, and longer-term trials and meta-analyses are needed. In such studies the outcome will depend on factors such as the age of the subject, relation to the menopause for women, initial dairy intakes and so on12. Intervention studies have, however, reported positive associations between increase in dairy food intake and BMC or BMD, and reductions in bone turnover markers13,14. On the whole, there is support for favourable effects of dairy on measures of bone health in adults3.
Fracture risk
With respect to fracture risk, while there are some inconsistencies and differences between different dairy products, overall, observational studies report beneficial or neutral associations. The differences may be due to heterogeneity in the study designs, duration, participants’ age, and other confounding factors such as vitamin D status and physical activity. Differences in usual dairy intake, both types and amounts, between countries and population groups may also be a factor. For milk, a meta-analysis of prospective cohort studies published in 2011, found no overall association between adult milk intake and hip fracture risk in women; insufficient data was available in men15. However, the data on women were disproportionately influenced by one study from Sweden; when the authors excluded this study from the analysis there was a marginally significant 5% lower hip fracture risk for each glass of milk consumed per day (200ml – 250ml). A subsequent publication in 2014 utilising data from the same Swedish cohort of 61,000 women but with a longer follow up (around 20 years) found fermented milk products (yogurt and other soured milk products) and cheese consumption were associated with a significant decrease in fracture incidence16. However, high intakes of milk (three or more glasses/day; more than 600ml/day) were associated with increased fracture rate. It is worth noting that when the dietary questionnaires were performed (1987–90 and 1997) milk in Sweden was fortified with high dose of vitamin A; such levels of vitamin A intake have been linked to an increased risk of fracture. Subsequently, two large observational studies of US men (43,306) and women (80,600) followed for up to 32 years report that each glass of milk consumed per day (240ml) was associated with an 8% lower risk of hip fracture17. Yogurt consumption in the cohorts was low and not associated with risk, and a suggestive association was found for cheese in women only. Interestingly, the reduced fracture risk with milk could not be explained by the intake of calcium, vitamin D and protein in the milk suggesting that other nutrients and / or interactions within the dairy matrix were involved in the effect on skeletal health.
Bringing together all the observational studies, a meta-analysis published in 2018 found that in both men and women, yogurt and cheese consumption were associated with reduced hip fracture risk18. This equated to a 32% lower risk between the highest and lowest cheese consumers and a 25% reduced risk between the highest and lowest yogurt consumers in cohort studies. There was no consistent relation between milk consumption and risk of hip fracture. Similar results were reported in a 2019 meta-analysis of studies of osteoporotic fractures in Europeans and Non-Hispanic whites from North America; the highest intakes of cheese and yogurt were associated with a reduced risk of fractures at any site (of 11% and 8%, respectively) whereas there was no relationship with milk19. For hip fracture specifically, there was no significant relation found with dairy foods. In another recent meta-analysis published in 2020 comparing the highest versus lowest category of dairy consumption, higher consumption of yogurt, but not milk or cheese, was associated with a lower (22%) risk of hip fracture20. A study of Finnish women has reported that milk avoidance (because of lactose intolerance) was associated with increased fracture risk21.
To date, fracture prevention trials have almost always been nutrient-based, primarily focusing on calcium and vitamin D supplementation; meta-analyses report a modest degree of effectiveness when calcium and vitamin D are combined22. However, the results from a recent food-based intervention trial with older people in long-term residential care in Australia, suggests that a dairy food-based approach has the potential for fracture prevention23. Sixty older people’s care facilities were randomised to provide residents with their usual menus or ones with extra milk, cheese and yogurt incorporated, increasing dairy consumption from 2 servings/day to 3.5 servings/day for two years. The intervention group with extra dairy had a 46% reduction in hip fractures, a 33% reduction in fractures overall and an 11% reduction in falls. Dairy foods are part of European guidance for postmenopausal women at risk from fractures due to osteoporosis24. The Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF) recommend a daily calcium intake of between 800mg and 1200mg along with sufficient dietary protein, and state that ideally this should be achieved through dairy products.
Potential dairy matrix mechanisms
The importance of calcium in bone development and maintenance is well established1,12. Milk and milk products make the largest contribution to calcium intake in the European diet. Few other foods naturally contain as much calcium, and dairy sources are some of the most bioavailable25. While it is sometimes assumed that supplementation with the same amount of calcium from different sources - e.g. milk, foods fortified with calcium and calcium supplements – have comparable effects on bone health, there is evidence of a beneficial ‘dairy matrix effect’26, 27. Dairy foods may have greater benefits than the equivalent calcium in the form of supplements. In adolescent girls, for example, it has been estimated that bone mineral density increases by up to 10% when 700mg extra calcium is provided as dairy foods, compared with an increase of 1% to 5% when the same quantity of calcium is given as a supplement28. Similarly, using cheese to increase calcium intake in 10- to 12-year-old Finnish girls resulted in a greater increase in bone mineral density compared to either a calcium supplement or a calcium plus vitamin D supplement7. Another randomised controlled trial investigating the effect of dairy products providing 1,200mg calcium a day or an equivalent calcium supplement on markers of bone metabolism and BMD found that after 12 months, the dairy intervention group had greater improvements in pelvis, spine and total BMD than the calcium supplement group13.
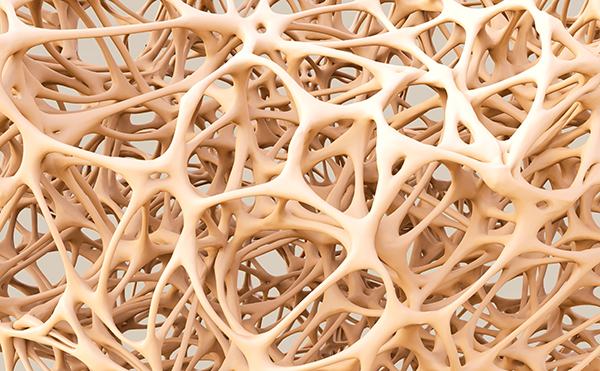
The greater benefits of dairy may be due to the presence of other nutrients in the dairy matrix which are important for bone health such as protein and phosphorus, and their interactions with calcium. Protein is essential for bone development in children and is needed for the maintenance of normal bones in adults since amino acids are required for the synthesis of intracellular and extracellular bone proteins. Protein provides the structural matrix of bone, making up 50% of bone volume. It is, of course, also involved in maintaining muscle mass and function; reduced muscle strength increases the risk of falls and therefore fractures. Older adults consuming a protein-restricted diet are at higher risk for bone loss and fractures, and sufficient protein intake is recommended in guidelines for maintaining skeletal health29-32. There has been some controversy around the adverse effects of high protein intakes, but it is now established that although a high-protein diet increases urinary calcium excretion this does not result in a negative skeletal calcium balance or bone loss29-34. In fact, research suggests higher protein intakes are beneficial to bone health, especially when calcium intake is also adequate31, 35. For example, in the US Osteoporotic Fractures in Men study, greater intakes of dairy protein were associated with a decreased risk of hip fracture36. Similarly, in healthy postmenopausal women, dairy protein intakes were positively associated with measures of bone strength and microstructure37. The potential mechanisms for this include protein enhancing calcium balance by stimulating intestinal calcium absorption, both directly and indirectly via an IGF1-vitamin D link.
Part of the explanation of the greater effectiveness of dairy calcium versus supplements may also be due to better absorption of calcium because of the presence of casein phosphopeptides and / or lactose in the dairy matrix7. Indeed, the casein micelle (a casein protein and calcium phosphate complex) evolved specifically to allow milk to transport large quantities of calcium. Fermented dairy products may additionally enhance calcium absorption through positive alterations in the gut microbiota38.
In addition to potentially larger effects, it has been suggested that the skeletal benefits of dairy calcium may persist longer than from calcium supplements30. In a study of 8-year-old French girls, the benefits of milk-extracted calcium phosphate on bone mass remained 3.5 years post supplementation4. This has not been the case after supplementation with calcium salts (such as citrate, malate or carbonate). Similarly, in an Australian study, in prepubertal children supplemented with ‘milk minerals’, benefits on BMC were still evident 12 months after discontinuation, compared with controls who received calcium carbonate39. Part of the explanation may lie in the favourable calcium to phosphorus ratio in milk. Phosphorus (as inorganic phosphate) is an important structural component of bone and an adequate intake is necessary for bone growth and development, and the maintenance of normal bones in later life29. Although a high intake, if accompanied by low calcium (in a ratio of about 4:1) may be deleterious to bone, the phosphorus to calcium ratio of milk (0.8:1) can enhance calcium balance by stimulating renal tubular reabsorption of calcium and lead to positive effects on bone40.
Other nutrients in milk and dairy foods are also involved in bone health including magnesium, potassium, vitamin K2 and zinc, along with vitamin D in fortified dairy1. There is increasing interest, for example, in the role that vitamin K2 (menaquinone) found in fermented dairy, particularly cheese, plays in bone mineralisation and reduced fracture risk41, 42. Fermented dairy foods such as yogurt and cheese are also a source of probiotics. A link between gut microbiota and bone exists which can be modified by probiotics to influence bone strength and bone mineral density43, 44.
Simply in terms of the quantities of ‘bone’ nutrients in dairy, it has been suggested that it is difficult to devise a diet that is ‘bone healthy’ without including three servings of dairy a day1. Increasingly, however, the scientific evidence indicates that the effect of dairy foods goes beyond the individual nutrients they contain, and that the nutrients and other bioactive components of the dairy matrix work in concert to help maintain bone health.
References
- Heaney RP. Dairy and bone health. J Am Coll Nutr. 2009; 28: 82S-90S.
- Weaver CM et al. The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporos Int. 2016; 27: 1281-1386.
- Rozenberg S et al. Effects of dairy product consumption on health: benefits and beliefs - a commentary from the Belgian Bone Club and the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases. Calcif Tissue Int. 2016; 98: 1–17.
- Huncharek M et al. Impact of dairy products and dietary calcium on bone-mineral content in children: results of a meta-analysis. Bone. 2008; 43: 312-321.
- van den Hooven EH et al. Identification of a dietary pattern prospectively associated with bone mass in Australian young adults. Am J Clin Nutr. 2015; 102: 1035-1043.
- Bonjour JP et al. Gain in bone mineral mass in prepubertal girls 3½ years after discontinuation of calcium supplementation: a follow-up study. Lancet. 2001; 358: 1208-1212.
- Cheng S et al. Effects of calcium, dairy product, and vitamin D supplementation on bone mass accrual and body composition in 10–12-y-old girls: a 2-y randomized trial. Am J Clin Nutr. 2005; 82: 1115–1126.
- Cadogan J et al. Milk intake and bone mineral acquisition in adolescent girls: randomized controlled intervention trial. BMJ. 1997; 315: 1255-1260.
- de Lamas C et al. Effects of dairy product consumption on height and bone mineral content in children: a systematic review of controlled trials. Adv Nutr. 2018; 10: S88–S96
- Black RE et al. Children who avoid drinking cow milk have low dietary calcium intakes and poor bone health. Am J Clin Nutr. 2002; 76: 675-680.
- Goulding A et al. Children who avoid drinking cow’s milk are at increased risk for prepubertal bone fractures. J Am Diet Assoc. 2004; 104: 250-253.
- Heaney RP. Calcium, dairy products and osteoporosis. J Am Coll Nutr. 2000; 19: 83S-99S.
- Manios Y et al. Changes in biochemical indexes of bone metabolism and bone mineral density after a 12-mo dietary intervention program: the Postmenopausal Health Study. Am J Clin Nutr. 2007; 86: 781-789.
- Moschonis G et al. The effects of a 30-month dietary intervention on bone mineral density: the Postmenopausal Health Study. Br J Nutr. 2010; 104:100-107.
- Bischoff-Ferrari HA et al. Milk intake and risk of hip fracture in men and women: a meta-analysis of prospective cohort studies. J Bone Miner Res. 2011; 26: 833-839.
- Michaëlsson K et al. Milk intake and risk of mortality and fractures in women and men: cohort studies. BMJ; 2014; 349: g6015
- Feskanich D et al. Milk and other dairy foods and risk of hip fracture in men and women. Osteoporos Int. 2018; 29: 385–396.
- Bian S et al. Dairy product consumption and risk of hip fracture: a systematic review and meta-analysis. BMC Public Health. 2018; 18: 165. doi: 10.1186/s12889-018-5041-5.
- Matia-Martin P et al. Effects of Milk and Dairy Products on the Prevention of Osteoporosis and and Osteoporotic Fractures in Europeans and Non-Hispanic Whites from North America: A Systematic Review and Updated Meta-Analysis. Adv Nutr. 2019: 10; S120-S143.
- Hidayat K et al. Systematic review and meta-analysis of the association between dairy consumption and the risk of hip fracture: critical interpretation of the currently available evidence. Osteoporos Int. 2020; 31: 1411-1425.
- Honkanen R et al. Lactose intolerance associated with fractures of weight-bearing bones in Finnish women aged 38-57 years. Bone. 1997; 21: 473-477.
- Yao P et al. Vitamin D and calcium for the prevention of fracture: a systematic review and meta-analysis. JAMA Netw Open. 2019; 2: e1917789.
- Iuliano S et al. Effect of dietary sources of calcium and protein on hip fractures and falls in older adults in residential care: cluster randomised controlled trial. BMJ 2021; doi.org/10.1136/bmj.n2364
- Kanis JA et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2019; 30: 3-44.
- Guéguen L & Pointillart A. The bioavailability of dietary calcium. J Am Coll Nutr. 2000; 19: 119-136.
- Thorning TK et al. Whole dairy matrix or single nutrients in assessment of health effects: current evidence and knowledge gaps. Am J Clin Nutr 2017: 105:1–13.
- Geiker NRW et al. Impact of whole dairy matrix on musculoskeletal health and aging – current knowledge and research gaps. Osteoporos Int. 2020; 31: 601–615.
- Kerstetter JE. Do dairy products improve bone density in adolescent girls? Nutr Rev. 1995; 53: 328-332.
- Bonjour JP. Protein intake and bone health. Int J Vitam Nutr Res. 2011; 81: 134-142.
- Bonjour JP et al. Dairy in adulthood: from foods to nutrient interactions on bone and skeletal muscle health. J Am Coll Nutr. 2013; 32: 251-263.
- Rizzoli R et al. Benefits and safety of dietary protein for bone health. A position paper from the International Osteoporosis Foundation and from the European Society for Clinical and Economical Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases. Osteoporos Int. 2018; 10.1007/s00198-018-4534-5. [Epub ahead of print]
- Darling AL et al. Dietary protein and bone health across the life-course: an updated systematic review and meta-analysis over 40 years Osteoporos Int. 2019; 30: 741-761.
- Kerstetter JE et al. Dietary protein and skeletal health: a review of recent human research. Curr Opin Lipidol. 2011; 22:16-20.
- Fenton TR et al. Causal assessment of dietary acid load and bone disease: a systematic review & meta-analysis applying Hill's epidemiologic criteria for causality. Nutr J. 2011; 10: 41-.64.
- Mangano KM et al. Dietary protein is beneficial to bone health under conditions of adequate calcium intake: an update on clinical research. Curr Opin Clin Nutr Metab Care. 2014; 17: 69-74.
- Langsetmo L et al. The association between protein intake by source and osteoporotic fracture in older men: a prospective cohort study. J Bone Miner Res. 2016 Dec 12. doi: 10.1002/jbmr.3058. [Epub ahead of print]
- Durosier-Izart C et al. Peripheral skeleton bone strength is positively correlated with total and dairy protein intakes in healthy postmenopausal women. Am J Clin Nutr. 2017; doi: 10.3945/ajcn.116.134676
- McCabe L et al. Prebiotic and probiotic regulation of bone health: role of the intestine and its microbiome. Curr Osteoporos Rep. 2015; 13: 363–371.
- Iuliano-Burns S et al. Skeletal benefits from calcium supplementation are limited in children with calcium intakes near 800 mg daily. Osteoporos Int. 2006; 17, 1794–1800.
- Bonjour JP. Calcium and phosphate: a duet of ions playing for bone health. J Am Coll Nutr. 2011; 30: 438S-448S.
- Beulens JW et al. The role of menaquinones (vitamin K2) in human health. Br J Nutr. 2013; 110: 1357-1368.
- Lundberg HE et al. Increased serum osteocalcin levels and vitamin K status by daily cheese intake. Int J Clin Trials. 2020; 7: 55-65.
- Rizzoli R. Nutritional influence on bone: role of gut microbiota. Aging Clin Exp Res. 2019; 31: 743-751.
- Rizzoli R & Biver E. Are probiotics the new calcium and vitamin D for bone health? Curr Osteoporos Rep. 2020;18: 273-284.